Abstract
Background Universal CAR-T (UCAR-T) using gene-editing techniques has attracted significant attention due to its prompt availability for patients. To date, there are only a few clinical case reports of universal CAR-T therapy for T-cell malignancies. Here, we explored the efficacy and safety of CD7-targeted UCAR-T (RD13-01) cells for relapsed or refractory (R/R) T-cell acute lymphoblastic leukemia (T-ALL) and T-cell lymphoblastic lymphoma (T-LBL) in a phase I clinical trial (NCT04620655).
Methods RD13-01 is an allogeneic, healthy donor-derived, and CRISPR/Cas9-edited anti-CD7 CAR-T cell product. RD13-01 consists of a CAR with a CD7-binding single-chain variable fragment (scFv), a 4-1BB costimulatory domain, CD3ζ signaling domain, a γc intracellular domain, in addition to an NK inhibitory (NKi) ligand containing an EC1-EC2 extracellular domain of E-cadherin fused to a CD28 co-stimulatory domain. The CAR and the NKi ligand are linked by an F2A self-cleaving peptide. Intravenous fludarabine (25-30 mg/m2/d), cyclophosphamide (300mg/m2/d) and etoposide (100 mg/m2/d) were given to all patients on Day -6 to Day -3 prior to CD7 UCAR-T cell infusion.
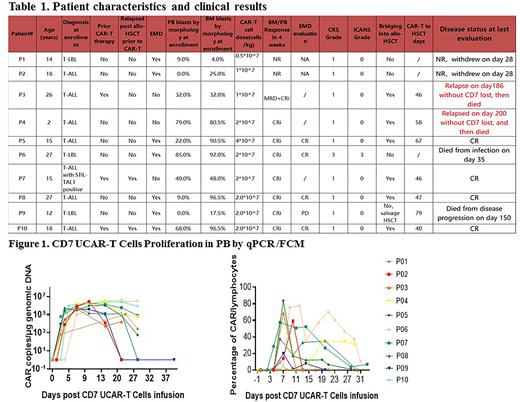
Results Between December 2020 and May 2022, 10 patients (7 males, 3 females), 7 with T-ALL and 3 with T-LBL were enrolled. Median patient age was 16.5 years (range: 2-27 years). Patients had a median of 4.5 (2-6) prior lines of therapies. Two patients relapsed from a previous allogeneic hematopoietic stem cell transplant (allo-HSCT) within 6 months. In addition, 3 patients who showed no response (NR) to prior autologous CD7 CAR-T therapy were also included. Patient characteristics are shown in Table 1. Four patients harbored high-risk genotypes including STIL-TAL1, TP53, BCR-ABL, and others. By morphology, the median bone marrow (BM) blasts at enrollment were 60% (4%-96.5%). Of the eight patients with peripheral blood (PB) blasts, the median blasts were 27% (9%-85%). At enrollment, 8 patients had extramedullary disease (EMD) including 3 with central nervous system (CNS) involvement (1 CNS-1, 2 CNS-3), 3 with diffuse involvement, and 3 had localized EMD.
The median transfection efficiency of the RD13-01 product was 64.6% (range: 59.0%-91.2%). A single dose of CD7 UCAR-T cells were infused to the first 3 enrolled patients at 0.5-1×107 cells/kg. Subsequently, 6 patients received a medium dose of 2×107cells/kg, and 1 received a high dose of 4×107cells/kg.
By the cut-off date of July 11, 2021, the median observation time was 153 days (range: 28-315 days). On day 28 post infusion, 8/10 (80%) patients achieved complete remission (CR) in BM/PB, and 7 of the 8 patients were minimal residual disease (MRD) negative. Notably, the 3 patients who had failed prior autologous CD7 CAR-T therapy achieved CR. The first enrolled 2 patients who received the low dose showed NR and withdrew on day 28. Among the 7 patients with EMD, 4 achieved EMD CR at the median day 30, 1 had progression disease (PD) and 2, with NR in BM, withdrew prior to EMD evaluation.
With a median time of 47 days (40-67 days) following infusion, 6 patients in CR (including 1 MRD +CR) underwent consolidation allo-HSCT, and 4/6 remained progression-free longest up to 315 days. However, 2/6 relapsed without CD7 lost on day 186 and day 200, respectively, and subsequently died. In addition, 1 CR patient died from bacterial infection on day 35. One PD patient received salvage transplantation and died from relapse on day 150.
Post infusion, 9/10 patients experienced grade I cytokine release syndrome (CRS) and 1/10 had grade 3 CRS. Only 1 patient with CNS-3 experienced grade 3 neurotoxicity.
By qPCR, CD7 UCAR-T cells reached a median peak level of 1.43×106 copies /μg genomic DNA (1.11×105~4.33×106)copies /μg genomic DNA, which occurred on day 12 (7-24 days). The median peak of circulating CD7 UCAR-T was 47.6% (0.01%~83.9%) occurring on day 7 (6-19 days), as measured by flow cytometry (Figure.1).
Conclusions Our phase I trial showed that the allogeneic "off-the-shelf” RD13-01 product was safe and dose-dependently effective in treating patients with heavily pretreated T-ALL/LBL, including those with EMD and prior allo-HSCT, those who already failed autologous CD7 CAR-T therapy, and who could not manufacture autologous CAR-T from the patient's own PB due to high blasts in PB and those with rapid disease progression. Long-term observation and more patients are needed to further evaluate the safety and efficacy of CD7 UCAR-T cells.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal